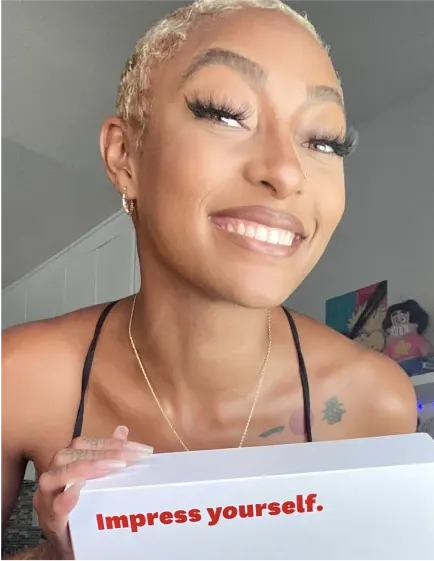
Backed by Dentsply Sirona, the world’s largest manufacturer of professional dental products, we’re making it easier for everyone to get the smile of their dreams—and gain the confidence they deserve.


A smile you can trust
Featured In
The Company that’s Changing the At-Home Dental Industry
Warby Parker, Glossier, and Beats by Dre all rolled up into a dental product
Whenever you notice a celebrity’s standout smile, there’s a good chance Dr. Jon Marashi is the cosmetic dentist responsible for their incredible teeth
Byte ’ s clients are consistently satisfied.
Day or Night Plans
Choose an aligner plan that’s right for you.
How Byte works
At-home impressions

Shipped straight to you. With easy instructions, it only takes a few minutes. Free return shipping.
Dentist Reviewed Aligners

We use your impressions to design a personalised treatment plan reviewed by an Australian registered dentist.
Track your progress

Watch your smile transform with access to your treatment plan through the MyByte app.
Byte Triple Lead

Our Guarantee
Your smile, for life.
You own your smile, and you should own it forever, so let’s guarantee it. If your smile moves out of alignment after you’ve completed your Byte treatment and followed post-treatment requirements like wearing a retainer, we’ll help get it back at no additional cost. See Guarantees for details
HyperByte™
Fast treatment times. Period.
With our exclusive HyperByte device included with each aligner plan, you get fast and comfortable treatment for a smile you love. ³
Dentist Reviewed Aligners
Your treatment plan is reviewed by an Australian registered dentist.
Our dedicated Customer Care Team is here to support you throughout your Byte journey.
Retainers coming soon

Looking for retainers?
Byte Retainers are currently only available with Byte aligner treatment, but they’ll soon be available for purchase on their own. Sign up now to get word on when you can order your own custom Byte Retainers designed just for you!




With so many shoutouts from raving fans, it’s hard to keep track, but we do our best.



Why Byte is better
DESCRIPTION
HyperByte® included
HyperByte, our exclusive high frequency vibration device, is included in every aligner kit. With just 5 minutes of use a day, the Hyberbyte assists with the seating of your aligners and facilitates better tooth movement.
Australian Dentist Reviewed
Byte’s clinical team will use your impressions to design a personalised treatment plan and create clear aligners just for your teeth.
First set of retainers for free
You’ll receive a free set of retainers with your Byte aligners. If you’re enrolled in the Byte Protection Program, you’ll automatically get a new set of retainers.
First bottle of premium whitening free
You get a bottle of BrightByte with your aligner purchase. BrightByte is a 3-in-1 foam cleanser, whitener, and breath freshener that works perfectly with your Byte aligners.
5 month average treatment time
While traditional braces often take over a year, the average treatment plan for our All-Day aligners is about 5 months,1 and our Byte at Night aligners is 6 months!2 Every smile is unique, so individual results may vary.
Clear and discreet
No more inconvenient appointments! You can straighten your teeth from the comfort of your home with our easy-to-use app and access to your clinical team 5 days a week.
Lifetime guarantee
If your teeth move out of alignment after you complete your initial treatment, we'll provide new aligners and help correct any misalignment issues at no additional cost.3
Legacy of trust
Byte is backed by Dentsply Sirona, the world's largest manufacturer of professional dental products—a brand trusted by dentists for over a century.
Guaranteed for life
Guaranteed for life.

We guarantee the work as long as you own your smile. If your smile moves out of alignment after you’ve completed Byte treatment (and followed post-treatment requirements like wearing a retainer), we’ll help get it back for free. See Guarantees for details.
Smiling Reviews
0 rating out of 0 reviews**
Reviews may include ones where known purchasers were given free product in exchange for their honest opinion.
Placeholder content lotem ipsum dolor sit adipisicing eli nesciunt autem, autem nulla consectetur content...
Placeholder content lotem ipsum dolor sit adipisicing eli nesciunt autem, autem nulla consectetur content...
Placeholder content lotem ipsum dolor sit adipisicing eli nesciunt autem, autem nulla consectetur content...
Placeholder content lotem ipsum dolor sit adipisicing eli nesciunt autem, autem nulla consectetur content...
Placeholder content lotem ipsum dolor sit adipisicing eli nesciunt autem, autem nulla consectetur content...
Placeholder content lotem ipsum dolor sit adipisicing eli nesciunt autem, autem nulla consectetur content...

